A new article by Qaisar, Qayum and Muhammad made me think about links between severe forms of asthma and some ALS forms.
Indeed this has already been questioned by scientists.
There are only a few studies addressing skeletal muscle function in patients with moderate to severe asthma.
Asthma is the result of chronic inflammation of the conducting zone of the airways (most especially the bronchi and bronchioles), which subsequently results in increased contractability of the surrounding smooth muscles. This among other factors leads to bouts of narrowing of the airway and the classic symptoms of wheezing. The narrowing is typically reversible with or without treatment. Occasionally the airways themselves change.
Patients with asthma have diminished activity patterns, leading to deleterious physiologic alterations and ultimately impaired functional capacity. Moreover, they may use corticosteroids during periods of disease exacerbation.
Yet patients with asthma who use systemic corticosteroids present a decrease in respiratory muscle strength. The use of high doses of glucocorticoids causes atrophy and loss of muscle strength, a condition known as steroid myopathy.
An effective pharmacological intervention in asthma remains elusive, partly because molecular mechanisms dictating muscle decline in asthma are not known.
The authors of this new article about the relation between asthma and muscle wasting, investigated the potential contribution of skeletal muscle sarcoplasmic reticulum Ca2+ ATPase (SERCA) to muscle atrophy and weakness in asthmatic patients.
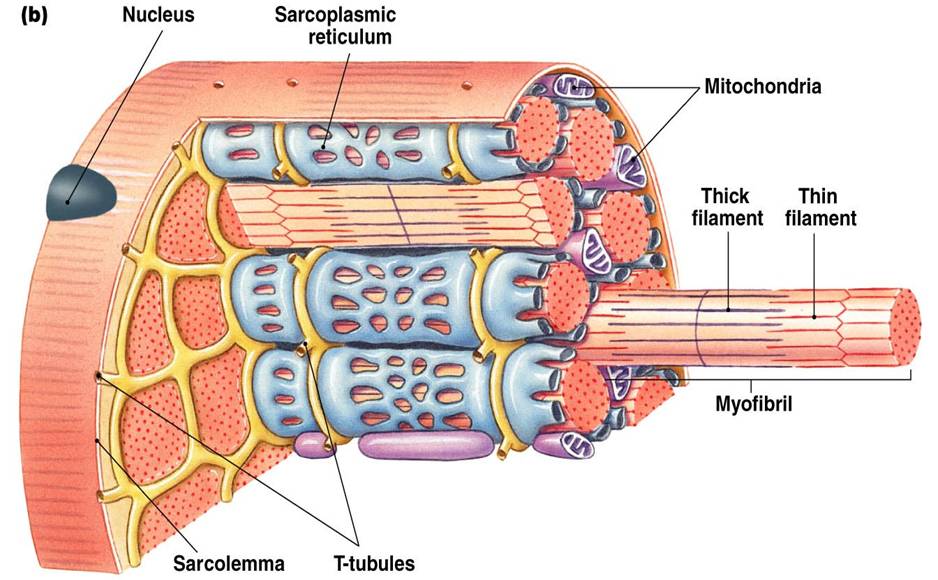
SERCA resides in the sarcoplasmic reticulum within myocytes. The sarcoplasmic reticulum is a membrane-bound structure found within muscle cells that is similar to the endoplasmic reticulum in other cells. The main function of the sarcoplasmic reticulum is to store calcium ions (Ca2+). Calcium ion levels are kept relatively constant, with the concentration of calcium ions within a cell being 10,000 times smaller than the concentration of calcium ions outside the cell.[
SERCA transfers Ca2+ from the cytosol of the cell to the lumen of the sarcoplasmic reticulum. This uses energy from ATP hydrolysis during muscle relaxation.In addition to its calcium-transporting functions, SERCA also generates heat in brown adipose tissue and in skeletal muscles
Quadriceps muscle biopsies were taken from 58 to 72 years old male patients with mild and advanced asthma and the SERCA activity was analyzed in association with cellular redox environment and myonuclear domain size.
Maximal SERCA activity was reduced in skeletal muscles of mild and advanced asthmatics and was associated with reduced expression of SERCA protein and upregulation of sarcolipin, a SERCA inhibitory lipoprotein.
Sarcolipin is an important mediator of muscle based non shivering thermogenesis. It causes the sarcoplasmic reticulum Ca2+-ATPases to stop pumping Ca2+ ions but continue futilely hydrolysing ATP, thus releasing the energy as heat. Sarcolipin mediated heat production is very important for many organisms to maintain a warm body. In mammals thermogenesis by skeletal muscles is complemented by thermogenesis in the brown adipose tissue.
The authors also found downregulation of Ca2+ release protein calstabin and upregulation of Ca2+ buffer, calsequestrin in skeletal muscles of asthmatic patients. The atrophic single muscle fibers had smaller cytoplasmic domains per myonucleus possibly indicating the reduced transcriptional reserves of individual myonuclei. Plasma periostin and C-terminal Agrin Fragment 22 (CAF22) levels were significantly elevated in asthmatic patients and showed a strong correlation with hand-grip strength. These changes were accompanied by substantially elevated markers of global oxidative stress including lipid peroxidation and mitochondrial ROS production.
Agrin, a synaptically located protein, is a key player during initial formation and maintenance of neuromuscularjunctions (NMJ). During development, nerve cells approach muscle fibers and establish synaptic contacts defined as NMJ. Initially, the NMJ is small and weak, but if the contact is successful the connection is maintained and reinforced. Agrin induces and stabilizes clusters of AChRs at the NMJ, promotes synaptic maturation, and maintains the mature state of the NMJ.
C-terminal Agrin Fragment has been proposed as a novel biomarker for sarcopenia originating from the degeneration of the neuromuscular junctions. Manipulation of the agrin signaling path may therefore be a promising way to correct neuromuscular defects.
During development in humans, the growing end of motor neuron axons secrete agrin. When secreted, agrin binds to several receptors on the surface of skeletal muscle. The receptor which appears to be required for the formation of the neuromuscular junction (NMJ) is called the MuSK receptor (Muscle specific kinase). Elevation of MuSK signaling has improved motor performance and delayed denervation in ALS mice (Perez-Garcia and Burden, 2012).
Taken together, the scientists' data suggest that muscle weakness and atrophy in asthma is in part driven by SERCA dysfunction and oxidative stress. The data propose SERCA dysfunction as a therapeutic intervention to address muscle decline in asthma.
You can write me at contact at padiracinnovation.org

